In the year 2018, the number of new cancer cases in the EU was approximately 3.91million (non-melanoma skin cancer was not included) while the number of deaths reached 1.93 million. Breast cancer was the most prevalent in females and prostate cancer the most prevalent in males representing together approximately 1 million cases [1]. Given the incidence and survivorship of breast and prostate cancer, they represent an important health problem for European countries [2,3,4].
Breast and prostate cancer patients present psycho-social needs. Different studies showed that almost a third of cancer survivors experienced changes in their work situation after treatment [5]. While the patient-centered approach is fundamental for improving the Quality of Life (QoL) of cancer patients through rehabilitation and support, there are two main obstacles to using survivorship care plans often: 1) the feasibility of integration at different health levels and 2) the cost and resources required to develop and manage these plans [6]. To mitigate the current barriers to monitoring QoL in cancer patients, two resources have emerged as disruptors: smartphones and wearables. Smartphones are widely used with 76% of total mobile connections performed through a smartphone in 2018 [7]. Wearables have also been on the rise with an estimated 116 million wearables devices sales in Europe in 2017 [8]. An increasing number of people are monitoring their own health using these new technologies, however monitoring diseases like cancer still faces some barriers. An example is the extraction of usable data from wearables and interoperability with electronic health records. In addition, another important barrier to the adoption of this technology in health monitoring is the technology education gap between young and old generations [9]. Access to education, access to a healthcare system, as well as the quality of living conditions, are important factors for addressing the challenges of monitoring QoL after cancer treatment. An advanced technological solution such as ASCAPE will have to lower these barriers while also adhering to GDPR, to national data protection, privacy and ethical legislation. At the same time it will have to provide an effective means of assisting doctors help patients navigate the challenges of their disease, the side-effects of treatments and a host of other factors in the context of a diverse range of socioeconomic challenges within which it will need to operate and prove itself to be an effective Information and Communications Technology (ICT).
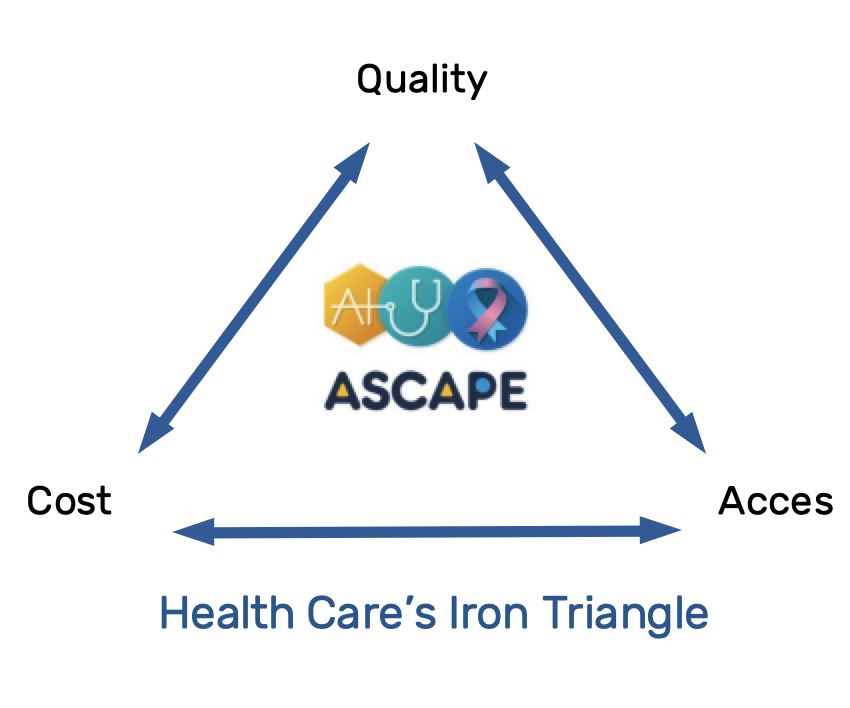
The Iron Triangle of Health introduced by William Kissisk reflects the paradigm of three opposing features in the healthcare system: healthcare access, delivery of quality and cost of care [10]. The idea of the Iron Triangle of Health is to demonstrate the connections between the three features, stating that any change in one of them will also impact the other two. Therefore, it would be almost impossible to improve access and quality while simultaneously reducing costs. For example, making healthcare accessible to more people without increasing costs necessarily needs to impact negatively the quality of care, or the quality of care could be improved but it will require the increment of cost or the limitation of access to healthcare. The concept is widely used in health policy and health economics with the general goal of keeping the balance under the inalterable constrain that increasing one feature will impact the other two assuming that there are not unnecessary services, inefficient processes and unfair prices.
The Iron Triangle concept is critiqued as proposing a rigid model that does not take into account costs and changing dynamics. Another major criticism is related to the impact of ICT in healthcare, and to the fact that the application of technology has already disrupted the model. The current development of technology, and AI in particular has already challenged the Iron Triangle concept and holds the promise that health care access and quality could be improved and cost reduced. Certainly, the development of artificial intelligence (AI) has already impacted the healthcare industry. AI is able to improve the quality of care by supporting better diagnosis, treatment and care. Moreover, AI can improve healthcare coverage by optimizing the resources and at the same time reducing cost. ASCAPE aims at disrupting the Iron-Triangle paradigm by developing AI models that will improve the Quality of Life (QoL) of cancer survivors while reducing costs to the healthcare systems and improving access to services.
ASCAPE has the opportunity to disrupt the Iron Triangle paradigm in different ways: 1) the ability to collect input from the patients and their devices directly which will lead to more data, and in turn increased AI results and quality of care, 2) less administrative effort for collecting data leading to lower cost of care and improving access of care by freeing time and human resources. Moreover, it is envisioned that the quality of the AI will improve. This improvement will lead to doctors making better recommendations to their patients, therefore improving quality of care and, in turn, reduced cost of care. Most importantly, ASCAPE will predict QoL issues sooner than with the current methods which will lead to better quality of care as well as cost of care, given that it will prevent downstream problems that burden greatly the health care systems. By achieving these goals, ASCAPE will disrupt the Iron Triangle of Health but most importantly, it will improve the QoL of cancer patients, which is the main goal.
Blog prepared by FCRB and Atos.
References
[1] J. Ferlay, M. Colombet, I. Soerjomataram, T. Dyba, G. Randi, M. Bettio, A. Gavin, O. Visser and F. Bray, “Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018,” Eur J Cancer, vol. vol. 103, p. 356–387, 2018.
[2] U. Dafni, Z. Tsourti and I. Alatsathianos, “Breast Cancer Statistics in the European Union: Incidence and Survival across European Countries,” Breast Care, vol. vol. 14, p. 344–352, 2019.
[3] International Agency for Research on Cancer IARC-WHO, “Europe Fact Sheets,” 2018. [Online]. Available: https://gco.iarc.fr/today/data/factsheets/populations/908-europe-factsheets.pdf.
[4] Crocetti, “Epidemiology of prostate cancer in Europe,” 2015. [Online]. Available:
https://ec.europa.eu/jrc/en/publication/epidemiology-prostate-cancer-europe.
[5] F. Mols, M. Thong, P. Vissers, T. Nijsten and L. v. d. Poll-Franse, “Socioeconomic implications of cancer survivorship: results from the PROFILES registry,” Eur J Cancer, vol. 48(13), p. 2037–2042, 2012.
[6] T. Albreht, R. Kiasuwa and M. Van den Bulcke, “European Guide on Quality Improvement in Comprehensive Cancer Control,” National Institute of Public Health and Scientific Institute of Public health, Ljubljana and Brussels, 2017.
[7] GSMA , “ The Mobile Economy Europe 2018 - The Mobile Economy,” 2018. [Online]. Available: https://www.gsma.com/mobileeconomy/europe/.
[8] Statista, “Wearables sales worldwide by region 2015-2022,” 2020. [Online]. Available:
https://www.statista.com/statistics/490231/wearabledevicesworldwide-byregion/.
[9] Y. H. Wu, S. Damnee, H. Kerherve, C. Ware and A. S. Rigaud, “Bridging the digital divide in older adults: A study from an initiative to inform older adults about new technologies,” Clin. Interv. Aging, vol. 10, p. 193–201, 2015.
[10] W. L. Kissick, Medicine's Dilemmas: Infinite Needs Versus Finite Resources, New Haven: Yale University Press, 1994.